Cervical plexus blocks are indispensable tools in anesthesia and pain medicine. They play a vital role in providing anesthesia and analgesia for various surgical and medical procedures involving the head and neck region [1]. When it comes to cervical plexus blocks, two distinct approaches have gained prominence: the superficial cervical plexus block and the deep cervical plexus block. When determining which type of block to perform, there are key differences, indications, techniques, and considerations for each approach, which are essential to aiding clinical practice.
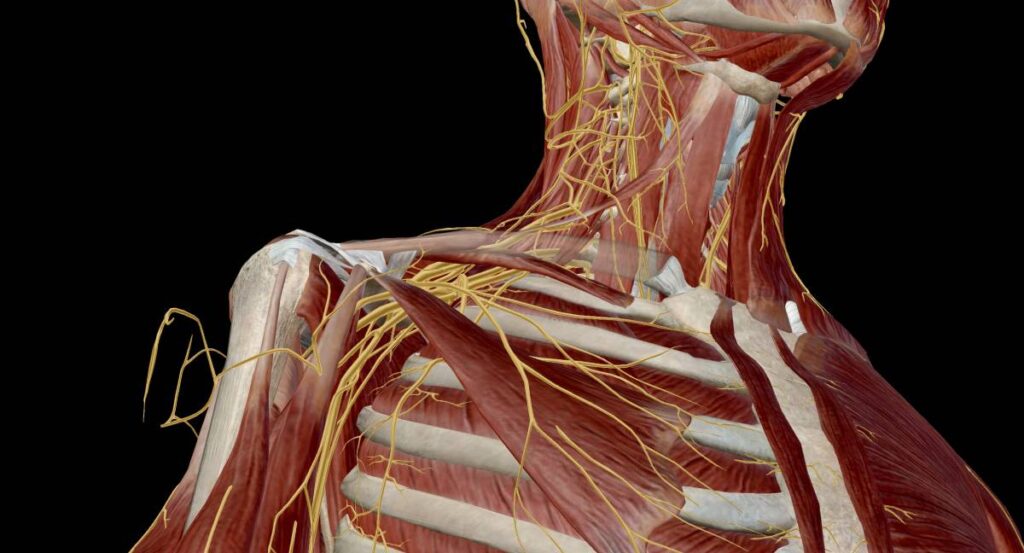
The cervical plexus consists of cutaneous sensory nerves originating from the cervical nerves C2-C4. These nerves innervate the skin and subcutaneous tissues of the head, neck, and posterior shoulders [2]. Superficial cervical plexus blocks are performed via subcutaneous injections at the border of the sternocleidomastoid muscle in the neck and can be guided with ultrasound [3]. These blocks are effective for analgesia for head and neck surgeries such as thyroidectomy, minimally invasive parathyroidectomy, tympanomastoid surgery, and even some types of craniotomy surgeries. They can also be used as adjuvant blocks for shoulder, clavicle, breast, or chest wall surgeries [2]. Superficial blocks are generally associated with fewer complications, which may include hematoma formation, infection, and inadvertent intravascular injection [4]. Furthermore, it is important that clinicians, when performing superficial blocks, aim the needle subcutaneously to avoid a deep block which can cause incidental complications [2].
The deep cervical plexus, on the other hand, is described as a paravertebral block which also targets cervical nerves C2-C4 [1,2]. These blocks not only block the superficial branches, but the deep branches of the cervical plexus as well. They are effective in providing anesthesia for surgeries involving deep structures within the neck such as carotid endarterectomies, thyroidectomies, parathyroidectomies, oral surgery, and maxillofacial surgery [5]. Deep cervical blocks carry a higher risk profile due to its proximity to vital structures. Complications may include intravascular injection, epidural or subarachnoid injection, and phrenic nerve palsy leading to diaphragmatic paralysis [2,3]. Thus, more advanced skills are required for these blocks and ultrasound is often utilized to safely and accurately visualize structures such as large vessels, nerves, and cervical fascia [2].
The decision to perform a superficial or deep cervical plexus block should be driven by the specific clinical scenario including the surgery to be performed, patient anatomy and characteristics, and the clinician’s proficiency. Each technique offers unique advantages and considerations. Overall, superficial cervical plexus blocks excel in providing quick and effective analgesia for superficial procedures and postoperative pain control and have a favorable safety profile. In contrast, deep cervical plexus blocks are essential for surgeries involving deeper structures, but often come with a higher risk profile. With the use of ultrasound, deep cervical blocks have become a common and relatively safe procedure [2]. Still, it is important to weigh the risks and benefits of cervical blocks with each clinical case as well as considering patient-specific factors.
References
1. Masters RD, Castresana EJ, Castresana MR. Superficial and deep cervical plexus block: technical considerations. AANA J. 1995 Jun;63(3):235-43. PMID: 7631578.
2. Kim JS, Ko JS, Bang S, Kim H, Lee SY. Cervical plexus block. Korean J Anesthesiol. 2018 Aug;71(4):274-288. doi: 10.4097/kja.d.18.00143. Epub 2018 Jul 4. PMID: 29969890; PMCID: PMC6078883.
3. Pandit JJ, Satya-Krishna R, Gration P. Superficial or deep cervical plexus block for carotid endarterectomy: a systematic review of complications. Br J Anaesth. 2007;99:159–69.
4. Pintaric TS, Hocevar M, Jereb S, Casati A, Novak Jankovic V. A prospective, randomized comparison between combined (deep and superficial) and superficial cervical plexus block with levobupivacaine for minimally invasive parathyroidectomy. Anesth Analg. 2007;105:1160–3.
5. Aunac S, Carlier M, Singelyn F, De Kock M. The analgesic efficacy of bilateral combined superficial and deep cervical plexus block administered before thyroid surgery under general anesthesia. Anesth Analg. 2002;95:746–50.