Labor epidurals have long been an essential part of modern childbirth practices, providing pain relief for countless women during labor and delivery. This medical advancement has not only transformed the birthing experience but also improved maternal and neonatal outcomes. In this article, we will explore the benefits, risks, and procedure of labor epidurals, shedding light on their role in contemporary childbirth.
What is a Labor Epidural?
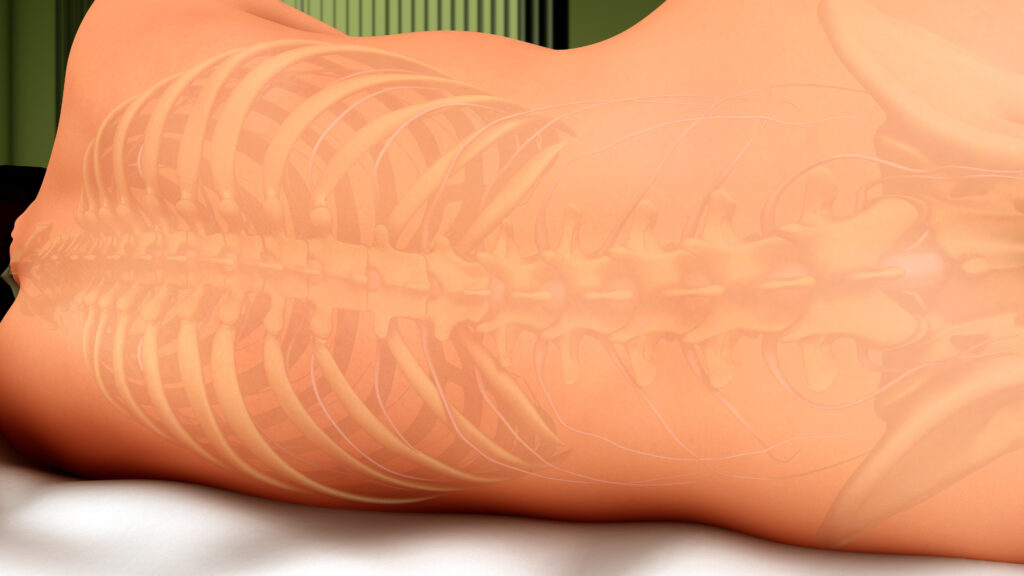
A labor epidural, also known as an epidural block, is a regional anesthesia technique used to provide pain relief during labor. By administering a combination of local anesthetic and analgesic medications into the epidural space, which surrounds the spinal cord, the procedure effectively numbs the lower part of the body. This allows the mother to maintain consciousness and actively participate in the delivery process while experiencing significantly reduced pain.
Benefits of Labor Epidurals
- Pain Relief: The primary benefit of a labor epidural is the significant reduction in pain experienced by the mother during labor. This relief can help reduce the need for systemic pain medications, which may have side effects for both the mother and baby.
- Improved Maternal Well-Being: The reduction in pain can lead to decreased stress, anxiety, and exhaustion, allowing the mother to better cope with labor and actively participate in the birthing process.
- Lower Rates of Instrumental Delivery: Studies have shown that labor epidurals can be associated with reduced rates of forceps or vacuum-assisted deliveries, which may lower the risk of injury to the baby.
- Enhanced Recovery: Epidurals can contribute to a more comfortable and rapid postpartum recovery, as the mother may be more alert and able to bond with her newborn sooner.
Risks and Side Effects
- Low Blood Pressure: Epidurals can cause a drop in blood pressure, which may require treatment with medications or fluids. Close monitoring is crucial to ensure the safety of both mother and baby.
- Incomplete Pain Relief: In some cases, the epidural may not provide complete pain relief, necessitating additional pain management measures.
- Slower Labor: Epidurals can sometimes slow down labor, increasing the need for oxytocin augmentation or leading to a longer second stage of labor.
- Potential Complications: While rare, some women may experience complications such as headache, fever, or nerve injury due to the epidural procedure.
The Procedure
The labor epidural procedure typically involves the following steps:
- Positioning: The mother is positioned either sitting up or lying on her side, with her back curved to optimize the placement of the epidural catheter.
- Sterilization: The healthcare provider cleans the skin in the lower back with an antiseptic solution to minimize infection risk.
- Local Anesthesia: A small injection of local anesthetic is given to numb the area where the epidural needle will be inserted.
- Catheter Placement: A thin, flexible catheter is threaded through a hollow needle into the epidural space. The needle is then removed, leaving the catheter in place.
- Medication Administration: The anesthetic and analgesic medications are administered through the catheter, which may remain in place for the duration of labor to provide continuous pain relief.
Labor epidurals have revolutionized the childbirth experience for many women by offering significant pain relief and improving maternal well-being. While there are potential risks and side effects, the benefits of epidurals often outweigh the drawbacks. It is essential for expectant mothers to discuss the option of a labor epidural with their healthcare providers to determine the best pain management plan for their individual needs.