Fascial plane nerve blocks are typically used to manage pain in the perioperative setting. In recent years, different types of fascial blocks have been described and there has been an increase in their clinical applications. First described in 2016 by Forero et al. the erector spinae plane (ESP) block is a relatively new nerve block that aims to deposit local anesthesia (LA) between the thoracic transverse process and erector spinae muscle (1). Compared to other regional anesthesia techniques, the ESP block has gained popularity due to the absence of a central neuraxial route, circumventing complications typically associated with spinal/epidural anesthesia (hematoma formation, total spinal anesthesia, hypotension, etc.) (2). For the last seven years, ESP blocks have been used to provide analgesia for a wide array of surgical interventions ranging from thoracic to spine surgery. Additionally, ESP blocks have also been used to manage chronic pain conditions, including complex regional pain syndrome and failed back surgery syndrome (1).
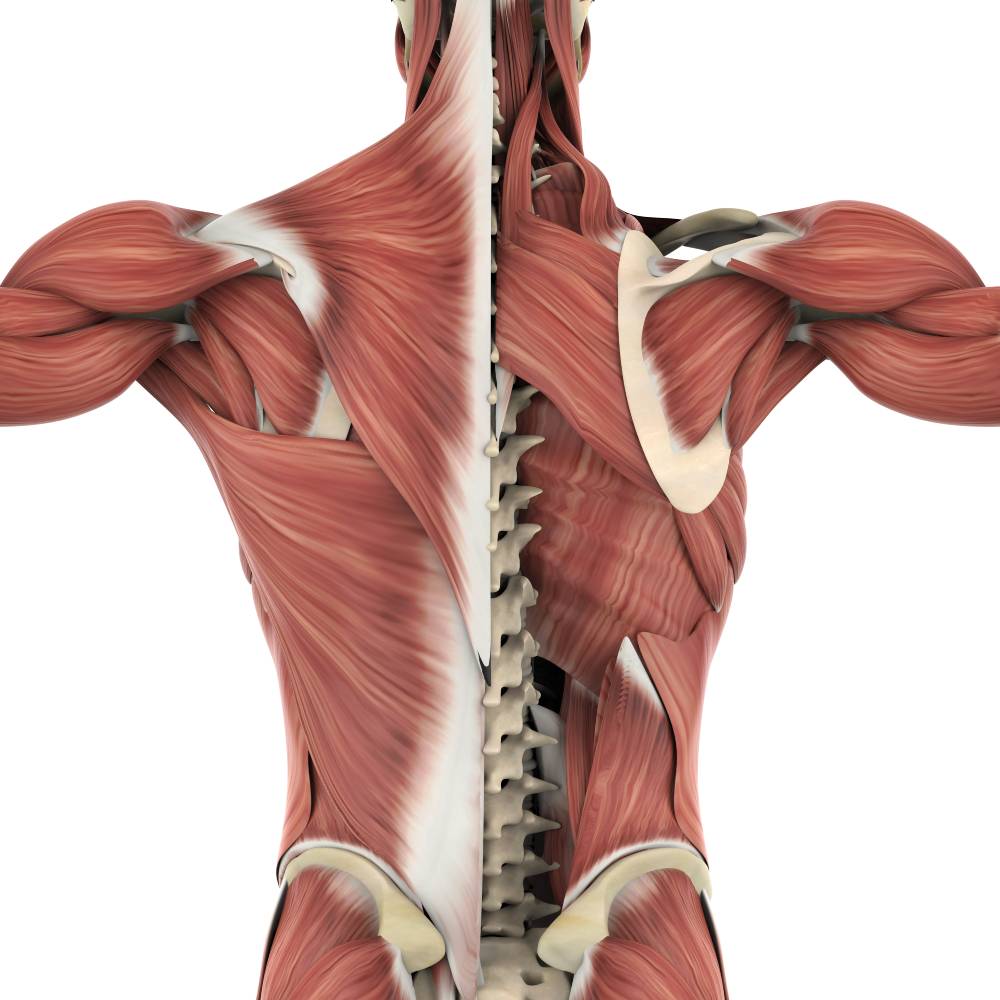
The erector spinae muscle runs the entire length of the spine and consists of the spinalis, longissimus thoracis, and iliocostalis muscles. The erector spinae plane lies in the paraspinal region anterior to the erector spinae muscle (2). To perform the block, LA is administered between the T5 and T9 thoracic levels. Using ultrasound guidance, LA is injected below the erector spinae muscle (deep needle approach) or between the rhomboid major muscle and erector spinae muscle (superficial needle approach). The deep needle approach is preferred as it allows LA to be deposited closer to the costo-transverse foramina and the origin of the dorsal and ventral rami of the spinal nerves. The erector spinae plane block works by blocking the dorsal and, to a lesser extent, the ventral rami of the T2–T9 spinal nerves (when LA is deposited between T5 and T9) (2). The clinical effects of ESP blocks result from the spread of LA into the paravertebral space through gaps in the paravertebral muscles, with 30 mL often resulting in adequate spread. Bupivacaine and ropivacaine are the most commonly used LAs (given their pharmacological properties and longer duration of action) which can be administered as either bolus injections and/or continuous catheter infusions (2).
In a 2019 narrative review published in the Korean Journal of Anesthesiology, several studies involving the use of the erector spinae plane block were analyzed to evaluate the efficacy of the technique (3). For example, Gürkan et al. evaluated the ESP block for postoperative analgesia in breast surgery. They compared 50 patients in two groups (ESP group and control group). It was found that total morphine consumption in the ESP group at 24 hrs was lower compared to the control group (5.76 ± 3.80 mg vs. 16.60 ± 6.92 mg), but there was no statistically significant difference between the groups in terms of numerical rating scale (NRS) pain scores. On the other hand, Krishna et al. evaluated the ESP block for postoperative analgesia in cardiac surgery. They compared 106 patients in two groups (ESP group and control group) and concluded that ESP block provided significantly better pain relief at rest (NRS were significantly lesser at all measured time points) and for a longer duration than the control group (8.98 ± 0.14 hours vs. 4.60 ± 0.12 hours) (2). Based on these studies, the ESP block appears to be a relatively effective form of analgesia in certain clinical situations. However, more randomized
controlled trials are necessary to establish the best indications of erector spinae plane block as an analgesic technique, in chronic, acute, and postoperative pain.
References
1. Saadawi M, Layera S, Aliste J, Bravo D, Leurcharusmee P, Tran Q. Erector spinae plane block: A narrative review with systematic analysis of the evidence pertaining to clinical indications and alternative truncal blocks. J Clin Anesth. 2021;68:110063. doi:10.1016/j.jclinane.2020.110063
2. King M, Stambulic T, Servito M, Mizubuti GB, Payne D, El-Diasty M. Erector spinae plane block as perioperative analgesia for midline sternotomy in cardiac surgery: A systematic review and meta-analysis. J Card Surg. 2022;37(12):5220-5229. doi:10.1111/jocs.17005
3. Kot P, Rodriguez P, Granell M, et al. The erector spinae plane block: a narrative review. Korean J Anesthesiol. 2019;72(3):209-220. doi:10.4097/kja.d.19.00012